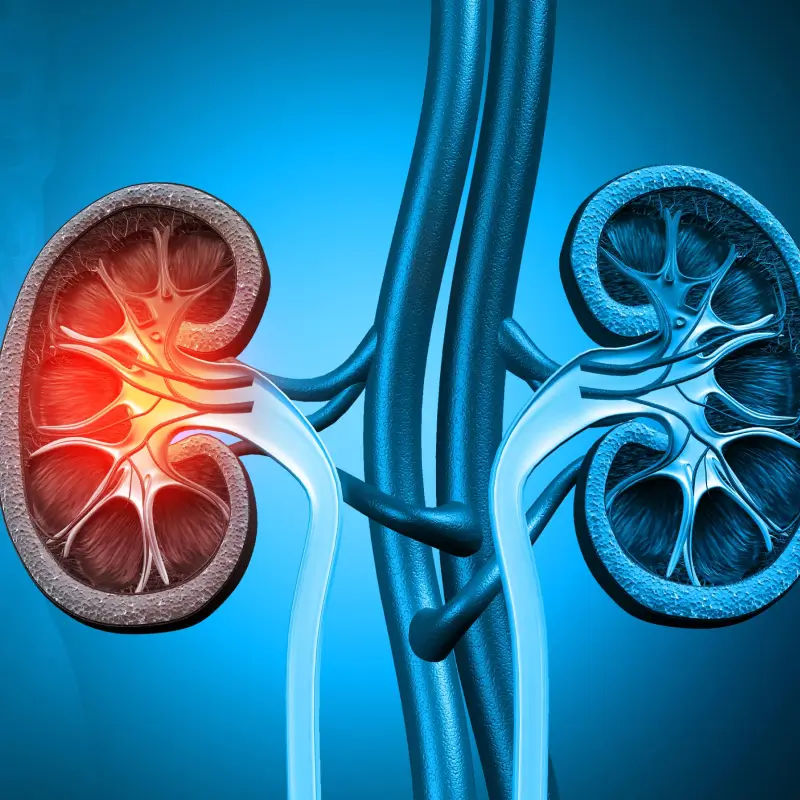
A donor nephrectomy is a surgical procedure performed to remove a kidney from a healthy donor for transplantation into a recipient suffering from end-stage renal disease (ESRD). This procedure allows patients with kidney failure to receive a functioning kidney, significantly improving their quality of life and survival. With advancements in surgical techniques, donor nephrectomy has become safer, minimally invasive, and highly effective.
Types of Donor Nephrectomy
There are two primary types of donor nephrectomy:
- Open Donor Nephrectomy – A traditional surgical approach where a larger incision is made to remove the kidney. This method is less common today due to the rise of minimally invasive techniques.
- Laparoscopic Donor Nephrectomy (Minimally Invasive) – A preferred technique that involves making small incisions to remove the kidney using a laparoscope. This approach leads to less pain, quicker recovery, and minimal scarring.
Procedure Steps
- Preoperative Evaluation – The donor undergoes comprehensive medical screening, including blood tests, imaging scans, and kidney function tests, to ensure they are a suitable match for donation.
- Anesthesia – The donor is placed under general anesthesia to ensure a pain-free experience during the surgery.
- Small Incisions (for Laparoscopic Nephrectomy) – Tiny incisions are made in the abdomen to insert a laparoscope (a thin, lighted tube with a camera) and specialized surgical instruments.
- Kidney Removal – The kidney is carefully dissected from surrounding tissues, blood vessels, and ureter. The main artery and vein are securely clipped before the kidney is removed through a small incision.
- Closure – The incisions are closed with sutures or surgical glue, allowing for faster healing and reduced postoperative discomfort.
Benefits of Donor Nephrectomy
- Improves the Recipient’s Quality of Life – A transplanted kidney from a living donor functions better and lasts longer than one from a deceased donor.
- Minimally Invasive Approach – Laparoscopic nephrectomy reduces pain, hospital stay, and recovery time.
- High Success Rate – Living donor kidney transplants have higher success rates compared to deceased donor transplants.
- Shorter Waiting Time for Recipients – Live donation helps patients avoid long waiting lists for deceased donor kidneys.
Risks and Complications
While donor nephrectomy is generally safe, potential risks include:
- Infection or Bleeding – As with any surgery, there is a risk of infection or bleeding, which is usually managed with antibiotics and careful post-operative care.
- Blood Clots – Prolonged immobility after surgery may lead to blood clot formation, which is why early movement and preventive measures are encouraged.
- Hernia at the Surgical Site – A small percentage of donors may develop a hernia at the incision site, which may require surgical correction.
- Temporary Fatigue and Discomfort – It is common to experience fatigue, mild pain, and discomfort in the initial weeks following surgery.
- Rare Cases of Long-term Kidney Function Reduction – Although rare, some donors may experience a slight decline in kidney function over time, which is why long-term monitoring is crucial.
Recovery and Postoperative Care
Recovery after donor nephrectomy is generally smooth, and most donors resume normal activities within a few weeks. Here’s what to expect:
- Hospital Stay – Most donors stay in the hospital for 1-3 days after surgery for close monitoring and pain management.
- Return to Normal Activities – Donors can resume light activities within 2-3 weeks, while full recovery usually takes 4-6 weeks. Strenuous activities and heavy lifting should be avoided during this period.
- Long-term Health Monitoring – Regular follow-up visits with a healthcare provider ensure that the remaining kidney is functioning properly and that there are no long-term health concerns.
- Healthy Lifestyle – Maintaining a balanced diet, regular exercise, and proper hydration is essential to support overall health and kidney function. Avoiding smoking, excessive alcohol, and high-sodium foods can also contribute to long-term well-being.
Who Can Be a Kidney Donor?
To be an eligible kidney donor, one must:
- Be in good overall health
- Have normal kidney function
- Be free from conditions like diabetes, hypertension, and kidney disease
- Be between the ages of 18-65
- Have a compatible blood type with the recipient
Conclusion
Donor nephrectomy is a selfless, life-changing gift that offers kidney failure patients a second chance at a healthy life. With modern surgical advancements, the risks are minimal, and donors can lead a normal life with a single kidney. If you are considering kidney donation, consult a transplant specialist to understand the process and its impact on your health.
FAQs
- Can I live a normal life with one kidney?
Yes, most kidney donors live healthy lives with one kidney, provided they follow a balanced lifestyle and regular medical check-ups.
- Is kidney donation painful?
With laparoscopic surgery, pain is minimal and manageable with medication.
- Will donating a kidney shorten my lifespan?
Studies show that kidney donors have similar life expectancy to non-donors and do not have an increased risk of kidney disease.
- How long does kidney donation surgery take?
The procedure typically takes 2-4 hours, depending on the complexity.
- Can I donate a kidney if I have high blood pressure?
Mild hypertension without organ damage may still allow donation, but a transplant specialist will determine eligibility.
- Will I need medication after donating my kidney?
No long-term medication is required, but donors need regular check-ups to monitor kidney function.